A Type One Diabetes Overview
Although many people have heard of type 1 diabetes (T1D), my experience is that very few people understand it. A lot of people I talk to also have misconceptions about T1D. I have done extensive research into T1D and have it myself. I was diagnosed at age ten, so I have just passed my 13-year anniversary.
Type 1 diabetes is just one of multiple types of diabetes. And yes, there are more than just two. T1D is also called insulin dependent diabetes mellitus. You may hear it referred to as just diabetes mellitus or insulin dependent diabetes. You may hear T1D called juvenile diabetes, but this is a misnomer because adults can develop the disease too. People also refer to it as diabetes without specifying the type, since that’s a lot shorter. If I just say diabetes in this post, I’m referring only to type 1.
Type 1 diabetes is an autoimmune disorder. That means that a person’s immune system attacks their own body cells. Specifically, the immune system attacks the beta cells in the pancreas. These cells sit in cell clusters called Islets of Langerhans. It’s a mouthful, but the important part is these are the cells that make insulin.
People aren’t usually born with T1D and it’s not just a disease of children. In fact, many in the community are pushing against phrases like “juvenile diabetes” because of how inaccurate they are. Adults make up a large portion of new diagnoses. In theory, the cause of T1D is a combination of genetic predisposition and environmental triggers that start the immune system on a path of self-destruction. However, neither the specific gene or triggers are known. T1D doesn’t have a strong inheritance pattern, unlike type 2 diabetes which runs in families.
Insulin acts like a bridge to bring glucose, the sugar your body uses as fuel, from your blood stream to your cells. Without insulin, sugar gets stuck in the blood and the cells in your body start to starve. Common symptoms are weight loss, extreme thirst, sweet smelling breath, frequent urination, hunger, nausea, tiredness, and vision changes. Hyperglycemia (high blood sugar) can become extremely severe and cause Diabetic Ketoacidosis, which happens when your body begins to break down its own tissues to feed its cells. This causes a build up of ketones and a rise in the acidity of the blood. This can be fatal and is unfortunately a common condition in new diabetics.
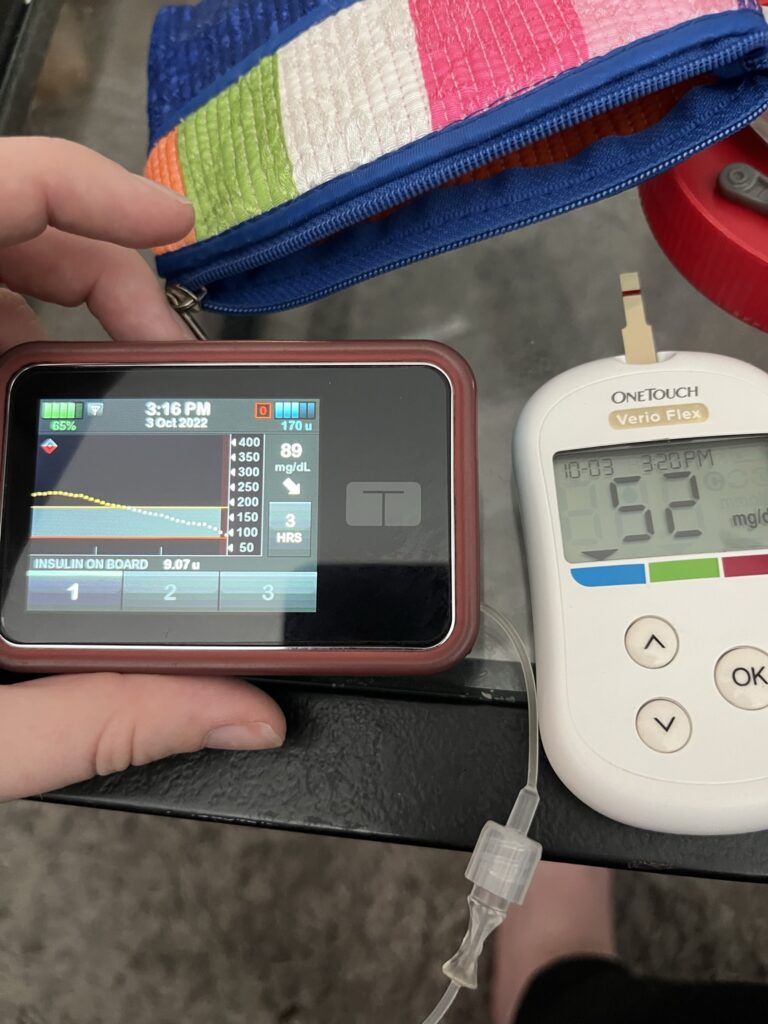
The treatment for T1D is multiple daily injections or a constant infusion of insulin. This is why you may hear a type one diabetic referred to as an insulin dependent diabetic. A diabetic administers insulin for three basic reasons. The first is as a daily long-acting injection or as a continues drip of short acting insulin from an insulin pump so that you always have a baseline level of insulin in your body. The second is when you intake carbohydrates. Diabetics learn to count the number of carbs in their food and calculate how much insulin they need to process those carbs. The last is blood sugar correction to keep high blood sugar down. Again, there is a unique calculation for each patient to find how much insulin they will need to take to bring a high blood sugar back into range.
Generally, the ideal blood sugar range is identified as 80-120 mg/dl (milligrams per deciliter, a tenth of a liter). Diabetics will struggle to stay in this range and may have a wider range of numbers they consider safe and manageable. I try to keep my blood sugar between 70-180 mg/dl. This is the range I know my body can handle and that I am realistically able to attain.
Damage to the pancreas from T1D also means that your body can’t regulate drops in blood sugar. In a healthy pancreas, low blood sugar will activate the hormone glucagon. This causes the liver to release stored sugar and regulates the sugar blood levels. Without this system, diabetics can experience low blood sugar (hypoglycemia) in addition to high blood sugar. Hypoglycemia can cause shaking, dizziness, odd or irritated behavior, confusion, sweating, fast heartbeat, weakness, tiredness, and anxiety. While most lows can be treated by eating something with sugar (like glucose tablets, juice, or candy) severe lows can happen and need emergency intervention with glucagon injections. Just like an out of control high, lows can be fatal.
There is currently no cure for T1D, although there are some new and exciting scientific developments in this area. An incurable, potentially fatal illness is a difficult thing to face, but I just celebrated my 13th “diaversary” (yes, we really do celebrate that!) and I’ve worked passionately to fund T1D research. We’re seeing the fruits of our labor, as scientists get better treatments, find prevention strategies, and get closer to a cure for type one diabetes.